This 54 year old Caucasian male patient was brought to the ER with altered mental status, and no preceding trauma or witnessed seizures. No history of fever, nausea or vomiting was reported. He had no visual symptoms, and past medical history was remarkable for bilateral congenital hip dislocation which required multiple surgeries. As an adult, he had multiple cardiac issues and had 4 coronary stents and a cardiac pacemaker implant.
He has a history of macrocephaly since early days of life, and he underwent a VP shunt at 4 months of age (1967). He does not remember having any shunt revisions until 2012 when he was found to have seizures and large cerebral ventricles on CT scan of his head. His programmable VP shunt was set at 170 mm Hg. He had shunt issues once again in 2014 and had a spinal tap once (details were unknown).
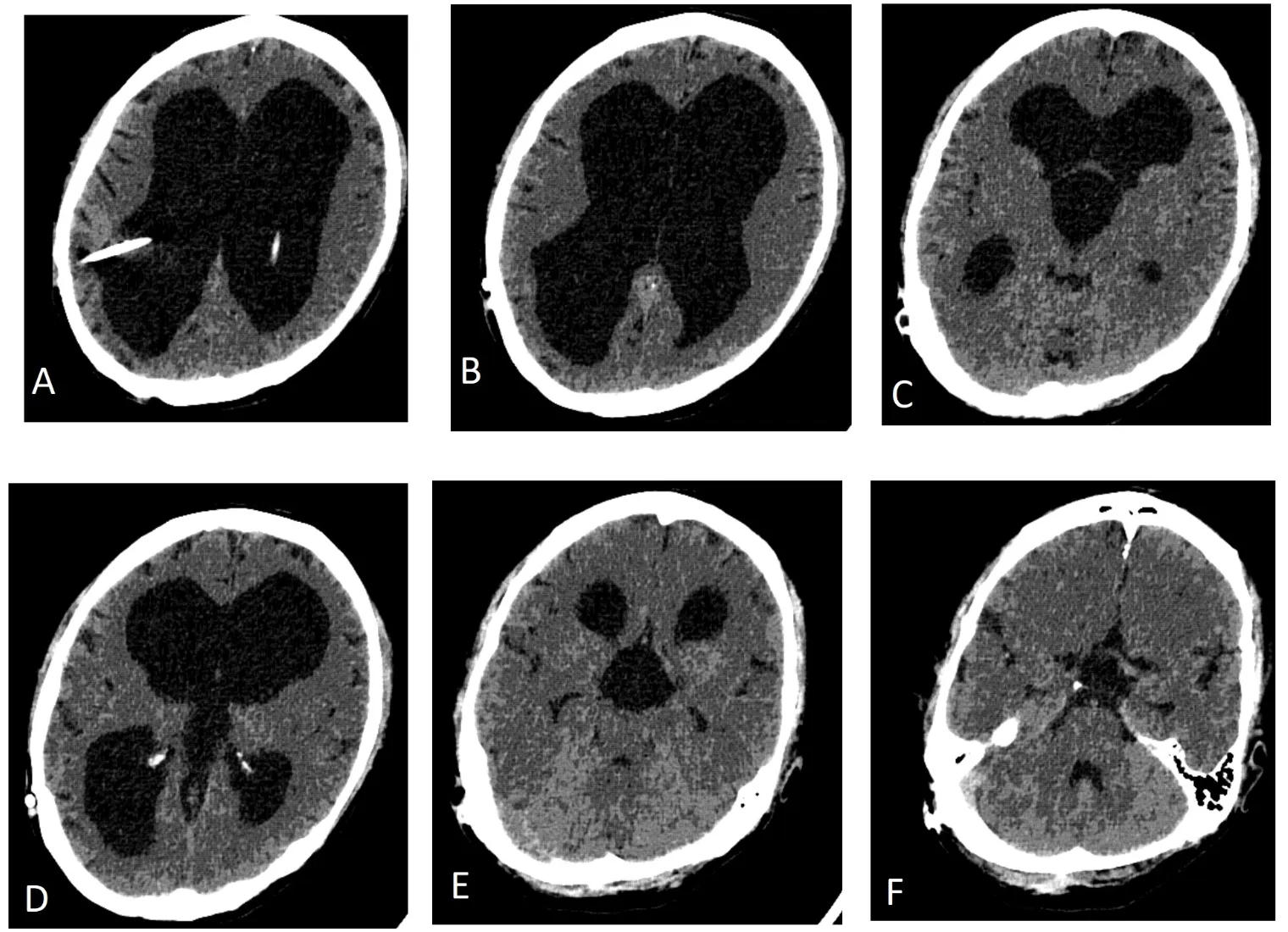
CT scan of head showed triventricular hydrocephalus with intact 4th ventricle, with widely patent foramen of Monro bilaterally. However, there was a slight hyperdensity of third ventricular CSF raising suspicion of a sequestered third ventricle, compared to CSF density in the lateral ventricles. Since there were no CT scans prior to this admission available for comparison, a CT ventriculogram was planned.
He recovered neurologically within 24 hours of admission slowly but remained extremely lethargic with no new lateralizing neurological deficits. It was decided to perform a CT ventriculogram to study CSF cells/ chemistry and culture, and assess the "trapped third ventricle", as his cardiac pacemaker precluded an MRI scan of brain with cine flow studies for CSF flow across the foramen of Monro and aqueduct.
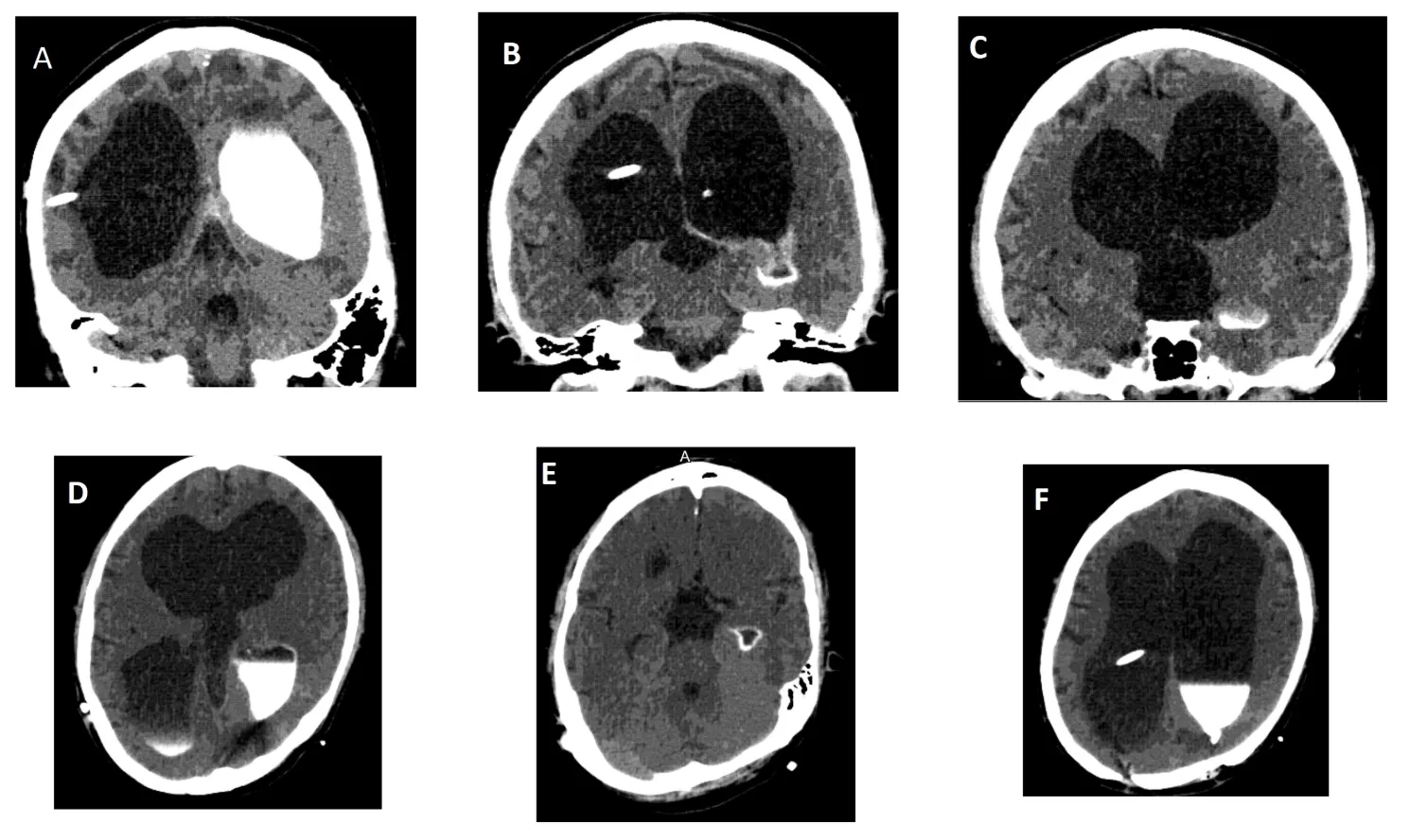
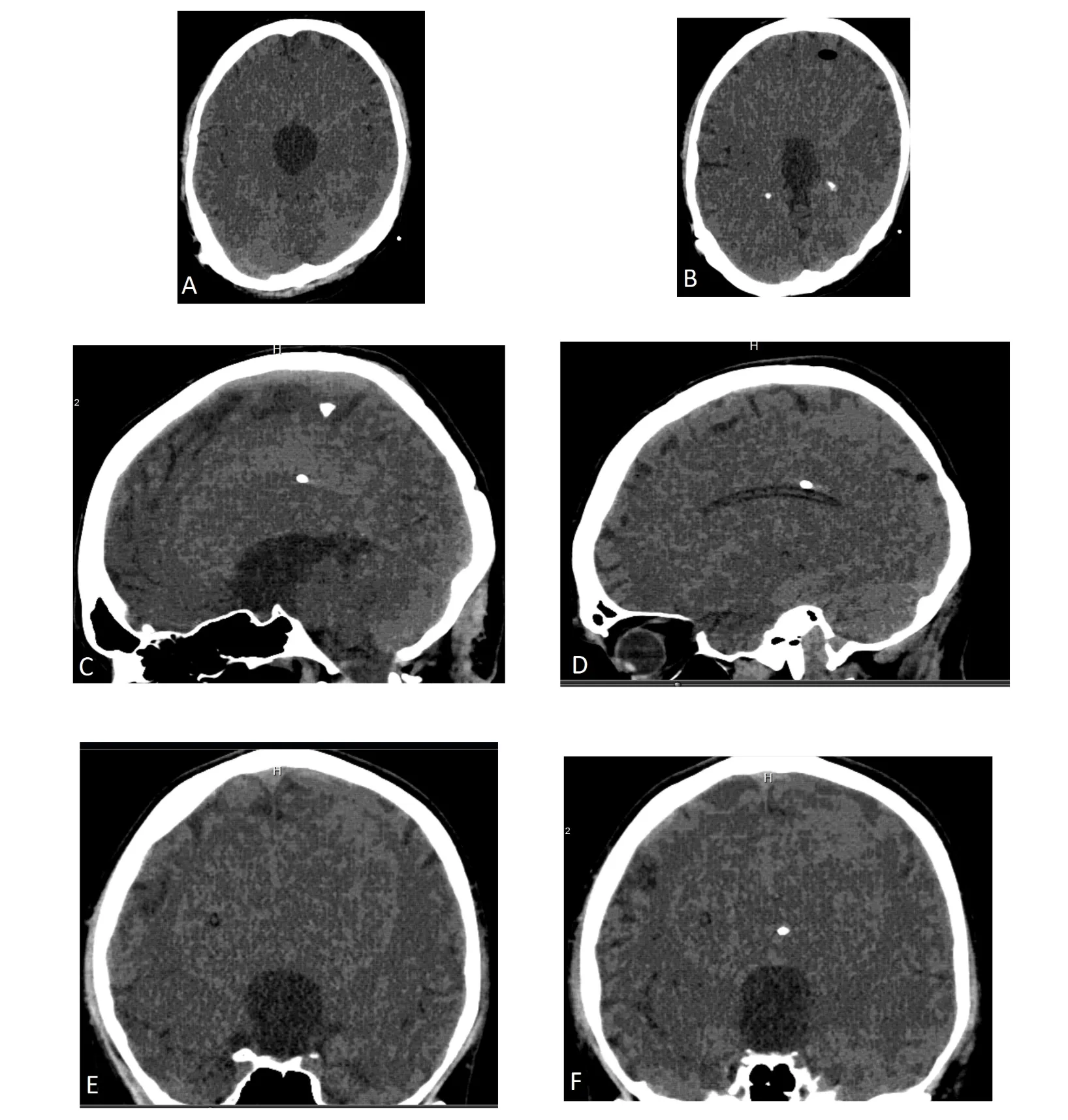
CT ventriculogram demonstrated a trapped third ventricle secondary to bilateral foramen of Monro obstruction or occlusion, with intact fourth ventricle. Figure 1 shows cranial CT with triventricular hydrocephalus and right VP shunt. The contrast dye placed in the frontal horn of lateral ventricle was not seen entering the third ventricle at all, even on follow up scans shown in Figures 2 and 3. No contrast egress was noted into the rounded enlarged third ventricle. Eventually the dye cleared off the lateral ventricles as demonstrated in Figure 4 done 24 hours after contrast injection. Given the fact that the patient improved neurologically and there was a possibility of arrested hydrocephalus, he was started on a higher dose of Keppra and he was discharged home at his neurologic baseline exam.
This case presents the dilemmas in sequestered or trapped third ventricle. If there was no contraindication of having a cardiac pacemaker, he would have undergone a non -invasive investigation such as cine flow MRI scan of brain. The literature review showed some unique and pathognomonic neurological symptoms and signs with sequestered third ventricle, which the patient did not have.
It is important to note that any reduction in the VP shunt setting would have led to an overdrainage subdural hematoma, and a trial of CSF drainage via EVD or externalization of existing VP shunt even would have probably led to an overdrainage of ventricular CSF. This case is a perfect example where any surgical intervention would have been riskier than masterly inactivity, and his subsequent head CT scans for active annual surveillance has shown no increase or decrease in ventricular size over the next three years to follow.